Role of MRI in Carbon Monoxide Diagnosis
Expanded use of MRI in Carbon Monoxide Diagnosis
The role of MRI in carbon monoxide diagnosis is rapidly expanding as imaging advances and extensive research have illuminated significant areas of brain damage. The most dramatic change in the diagnosis is the use of MRI in Carbon Monoxide diagnosis. Newer MRI protocols are for the first time, providing clear information about brain function. More significantly, the traditional structural imaging techniques have far greater resolution than they did a generation ago. While these improvements have only incrementally improved the radiological findings for other brain damage, it has changed the landscape for the use of the MRI in carbon monoxide diagnosis.
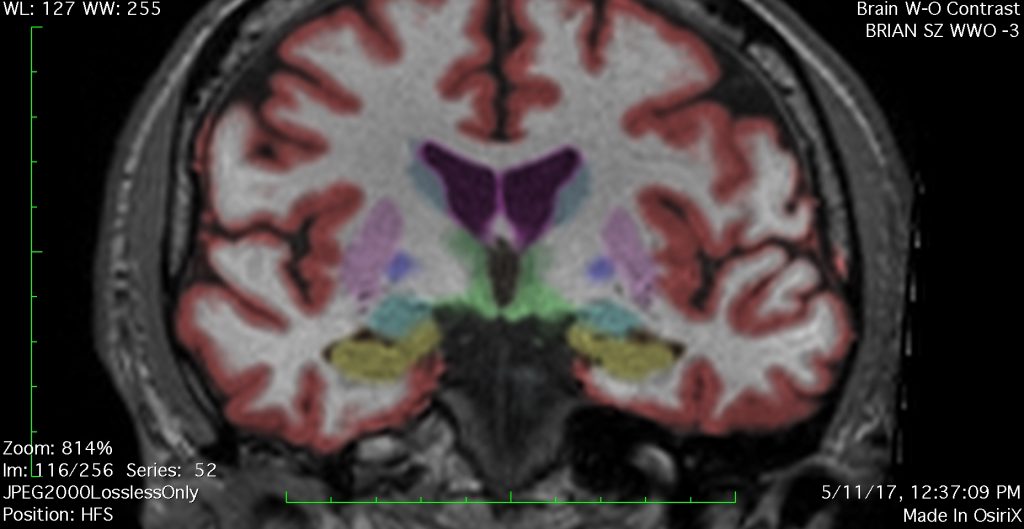
The importance of MRI in Carbon Monoxide diagnosis is increasing as new imaging protocols are developed. Also of importance is improved resolution found on 3T MRI. Shown here is a coronal image (front facing) on a NeuroQuant sequence.
Generally MRI and other diagnostic tools do not definitively diagnose brain damage after carbon monoxide. The exception is that lesions in certain areas of the brain are so specific for carbon monoxide that it may be the only thing on the differential diagnosis.
Carbon Monoxide Can Cause Ischemic Brain Damage
It is important to understand that CO poisoning starts as an ischemic event, where the initial damage is from hypoxia, insufficient oxygen to brain cells. More severe ischemic events can also be called anoxic, near total loss of oxygen to brain cells. Carbon monoxide takes the place of oxygen in the blood and thus brain cells can be asphyxiated if the hypoxia gets to severe.
Not all CO Brain Damage is Symmetrical
As the blood is circulated symetrically throughout the body, one might expect to see symmetrical brain damage on MRI as a result. But that ignores the science that hypoxia is the not only mechanism of brain damage in most of those who survive. In the most severe cases, where anoxia/hypoxia causes coma and death, older imaging techniques did tend to show bilateral lesions. When comatose CO survivors were being studied on CT, the primary finding was bilateral basal ganglia lesions, often in the globus pallidus.
But the bilateral nature of hypoxia is only a portion of the brain damage that occurs after CO poisoning. The bigger portion is the inflammatory/immunological response which goes on for days or weeks after the poisoning. The body senses CO as a poison and over reacts to this poison in destructive ways. As MRI technology improved, far more lesions were found and those lesions were just as likely to be one sided as bilateral.[1]
Understanding the Alphabet Soup of Carbon Monoxide Diagnosis
It may be helpful to explain what some of the abbreviations used when referring to diagnostic tools stand for. Neuroimaging and other modern diagnostic tools involve more than the MRI. They include the following traditional tools:
- CT – Computerized Tomography. An extremely valuable tool for head injury, less valuable for CO poisoning. It is the first imaging study that will be order in the ER in almost all cases of trauma, including CO poisoning. Its limitation is that it primarily identifies intracranial pressure events and large scale hemorrhage. Those are rare after carbon monoxide poisoning. http://subtlebraininjury.com/ct-after-concussion/
- MRI – The topic of this page. More below.
- EEg – a decades old technology that will identify electrical abnormalities in the cerebral cortex, but are often read as normal after CO poisoning. http://subtlebraininjury.com/eeg-after-concussion/
- PET Scan – Positron Emission Tomography. A decades old functional test, with limited availability and mediocre resolution. While the latest versions of PET scans are better than they were 20 years ago, they are not nearly as sensitive as the best MRI protocols at identifying the type of brain damage after a CO event. SPECT scans are more available but have even worse resolution. http://subtlebraininjury.com/pet-scan-after-concussion/
- Electronystagmography. One of the many valuable diagnostic tools for identifying dizziness, balance and vertigo. Typically administered by ENT doctors, otolaryngologists or neuro-otologists. These tests can be integral part of diagnosing the pattern of neurological deficits found in CO cases. http://vestibulardisorder.com/eng.php
- VEP – Visual evoked potentials. This is a test of the optic nerve transmission and be a key finding after brain damage, particularly CO caused brain damage.
MRI Protocols Used for Diagnosing CO Brain Damage
Each generation of MRI imaging gets better. Each time MRI resolution improves, new protocols are developed, more brain damage from carbon monoxide poisoning is identified. That doesn’t mean that the brain damage is getting greater. It just means that current state of the art can image more of the brain damage that has always been there. The smallest lesion a 3-Tesla MRI can see is approximately 1 mm. Thousands of axons can be damaged in an area that small and still not show up on even the best scanner used for clinical use today.
The state of the art MRI in 2020 includes the following sequences:
- T1 and T2 imaging. On T1 images, the cerebral spinal fluid (CSF) is black. On T2 images, the CSF is white. (T1 and T2 are not to be confused with 3T – which is short for 3-Tesla, which is a measurement of the strength of the magnet.)
- T2 Flair – This is a T2 image where the CSF is black, but other qualitative aspects of T2 are preserved. (Yes that gets confusing.)
- Axial, Coronal and Sagital views of each of the above. The best MRI’s are done in all three planes. Axial is looking down at the head, like a road map, with each successive slice moving lower. Coronal is looking straight at the face, with each successive slice going further back. Sagital is looking at the head from the side, with the slices going from one ear to another.
- DWI, diffusion weighted images. DWI is the most sensitive test for CO in the first 24 hours after the poisoning, but unfortunately is rarely done acutely. It is now most valuable for diagnosing ischemic strokes, but should be ordered in the ER as routinely as CT scans are ordered. It lacks any sensitivity more than 4 days after the ischemic event.
- DTI – Diffusion Tensor Imaging. DTI is a protocol used to identify damage to fiber tracts in the brain. This is the most researched advanced imaging protocol but it has been around for more than 15 years now and should be included in all brain damage studies.
- SWI and other Hemosidrin studies. SWI stands for susceptibility weighted sequences. Hemosidrin is the blood deposits that are left behind after a bleed. Hemosidrin studies have been around for most of this century but the SWI is far more sensitive than the GRE protocols that preceded it.
- Brain volume studies, most often Neuroquant. These studies measure the 3 dimensional volume of all brain studies.
- MRS – Magnetic Resonance Spectroscopy. This is a modern protocol that measure the metabolites within the brain.
- fMRI – This is a functional MRI than can see in real time, the type of brain function issues historically only seen on PET and SPECT scans. This tool offers far superior resolution to PET and is a real time test, where PET is not.
- Perfusion studies. These studies are functional tests that can identify blood perfusion issues in the brain.
Brain Volume Loss on MRI in Carbon Monoxide Poisoning
Though any given neuron is infinitely too small to be seen by even the most advanced MRI magnets, when millions of neurons and axons die in a given structure those structures become smaller. Brain atrophy can be seen on an MRI, even when the scanner can’t see specific areas of dead brain. NeuroQuant or other imaging software can show these losses statistically. But as important as the measured loss of brain matter is the neuroradiologists call of visible volume loss. Knowing a pathology in the shape or size of given brain structures is a subjective diagnosis that those who study carbon monoxide poisoning are best suited to see.
One subcortical area that volume loss is very easy to see if the hippocampus, as it is surrounded by temporal horns, which are cerebral spinal filled areas. When the hippocampus get smaller, the temporal horns get bigger. As they are water versus brain tissue, their enlargement is easy to spot. An experienced neuroradiologist should always look to the temporal horns to see if they are enlarged and based upon his subjective read of the adjacent structure, call hippocampal atrophy if it exists.
[1] Basal ganglia lesions following carbon monoxide poisoning RAMONA O. HOPKINS1,2,3, et. al., Brain Injury, March 2006; 20(3): 273–281.




